Your Insurance Company Has 100+ Oncology Nurses You Never Knew About
Insights from UnitedHealthcare California CEO, Steve Cain
You just heard three words that stopped your life cold: “You have cancer.”
Your doctor is talking, but you’re not really hearing anything. Something about oncologists and biopsies and treatment plans. You hang up. And then... what? Who do you even call?
Most people call their spouse, their mom, or their best friend. They spiral into Google searches at 2 AM. They stare at the MyChart results they can’t interpret.
Almost nobody calls their insurance company.
I get it. When I was diagnosed, the last thing I wanted was to navigate a phone tree while my world was falling apart. But after talking with Steve Cain, CEO of UnitedHealthcare California, I learned we’re missing something important.
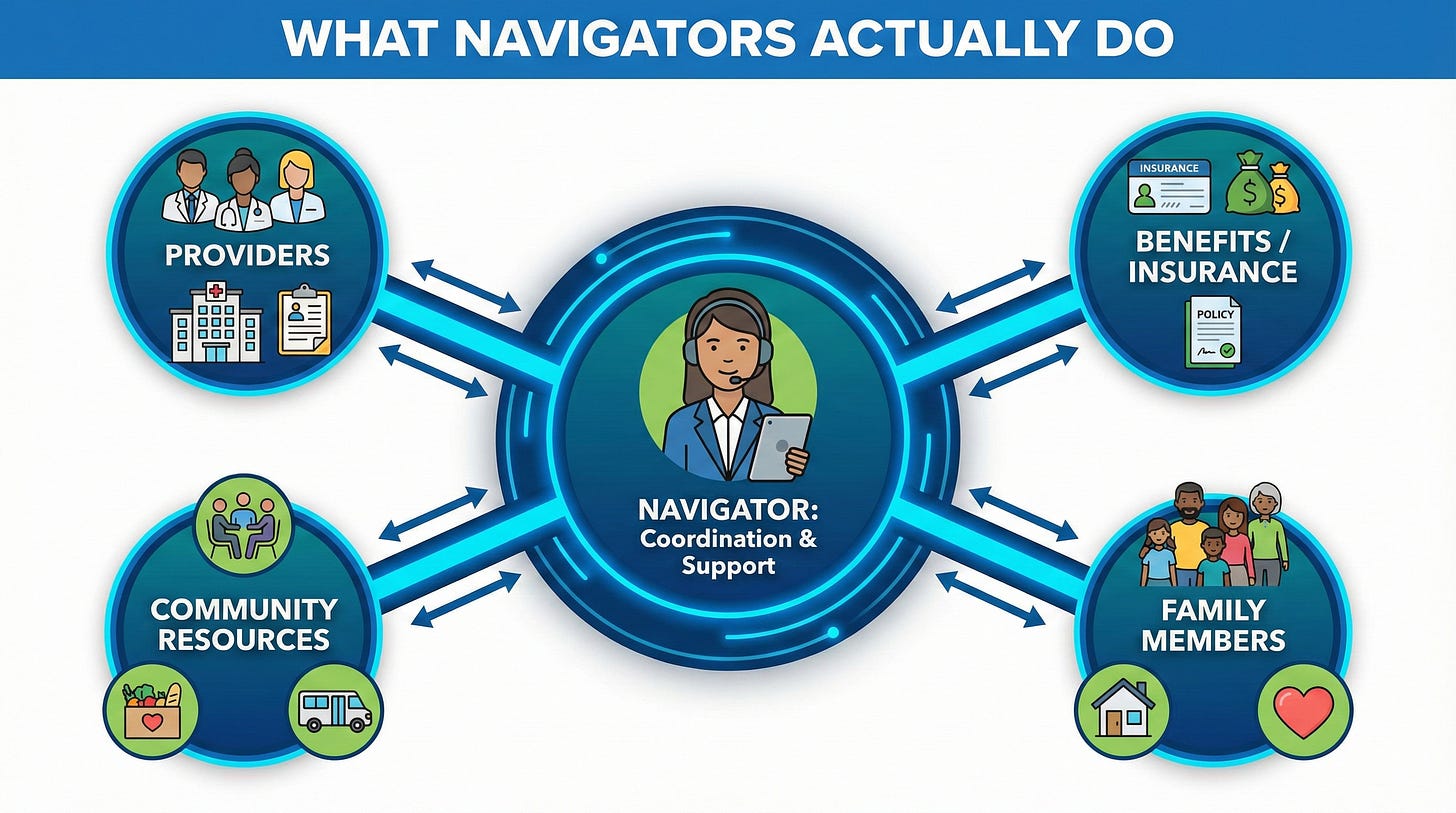
UnitedHealthcare has over 100 registered nurses with oncology experience whose entire job is to guide cancer patients through their treatment journey. One nurse, assigned to you, from diagnosis through survivorship. They coordinate across providers. They decode your benefit complexity when you’re in no state to read fine print. They even know about niche resources—like lymphedema specialists—that you won’t find on Yelp.
And yet, in the thousand-plus cancer patients and survivors I’ve talked to, exactly one person told me they got a call from a navigator right after diagnosis.
One.
The disconnect isn’t that these programs don’t exist. It’s that we don’t know to ask for them.
Two things you can do right now:
Save the phone number on your insurance card—and actually call it. The moment you get a cancer diagnosis, call that number and say: “I was just diagnosed with cancer. Do you have a navigator to help me?” Steve’s advice was blunt: “Call us. Get into the program. Allow us to help you.”
Remember: denied doesn’t always mean no. Most first denials occur because the insurance company didn’t receive the correct information from your provider. Before panicking, call your doctor’s office and ask them to review what was submitted. Often, it’s a paperwork problem, not a rejection of your care.
Cancer makes you feel alone. But there are people whose job it is to be in your corner—and they’re waiting for you to reach out.
In the full subscriber article, I break down exactly how payers use your claims data to trigger outreach, what navigators actually do (and how your family can call on your behalf), why “denied” is often just a paperwork gap, and the $0 copay initiative for screenings that could change when your cancer gets caught.
Listen to the full episode to hear Steve explain the prior authorization process and why he says the best thing you can do as a patient is “be relentless.”
Accessing UHC California Cancer Support
Cancer Support Program | UHCprovider.com
People can also call 866-936-6002