What if we could cut breast cancer diagnoses in half?
From Screening to Prevention: The Future Dr. Esserman Is Building
Dr. Laura Esserman doesn’t just want to find cancer earlier. She wants to stop it from happening at all.
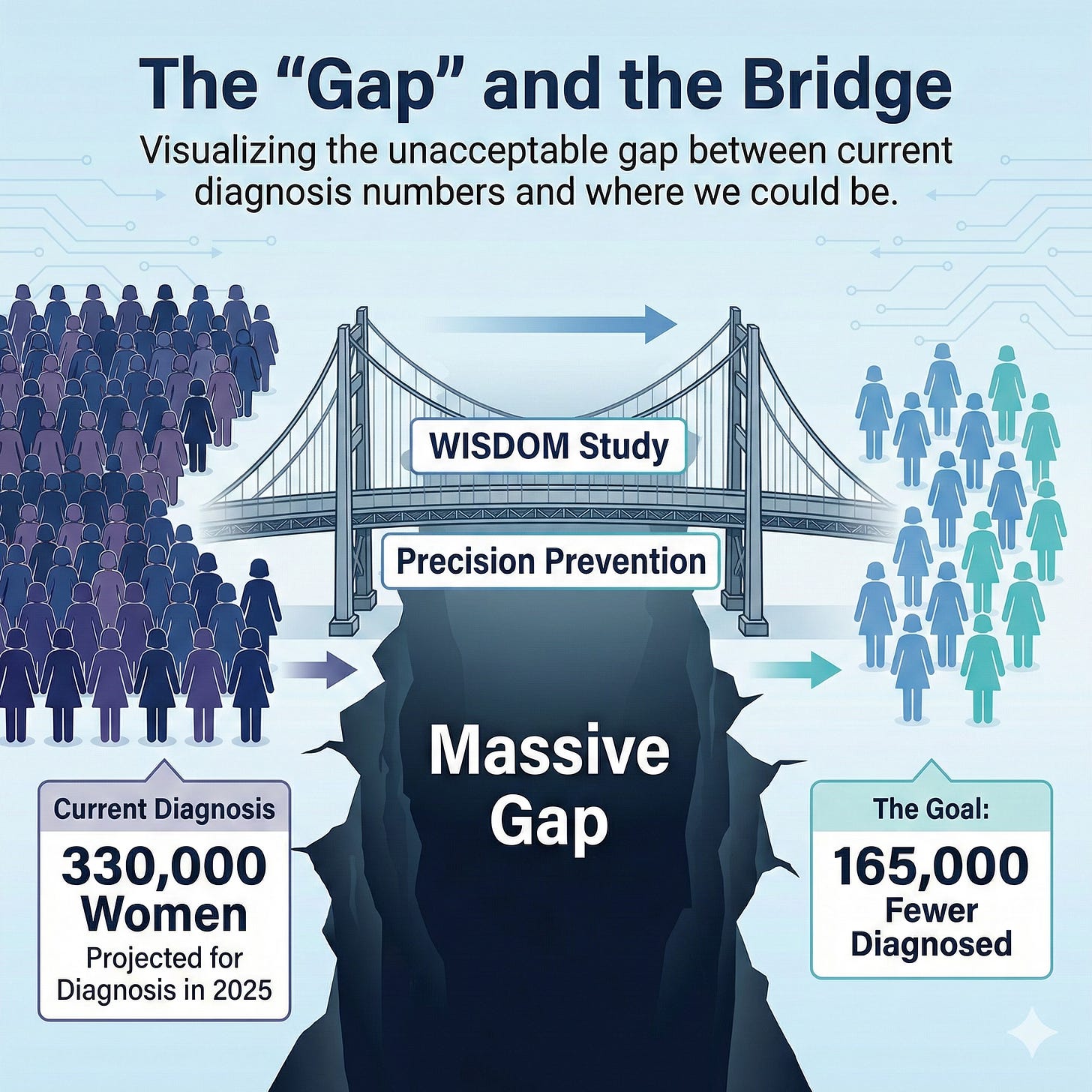
When she looks at the numbers—330,000 women diagnosed with breast cancer in 2025, up from 150,000 when she started her practice—she doesn’t see progress. She sees a gap. A massive, unacceptable gap between what we’re doing and what we could be doing.
“Why can’t we be trying to do things where we drop that number in half?”
It’s not a rhetorical question. She’s already building the answer.
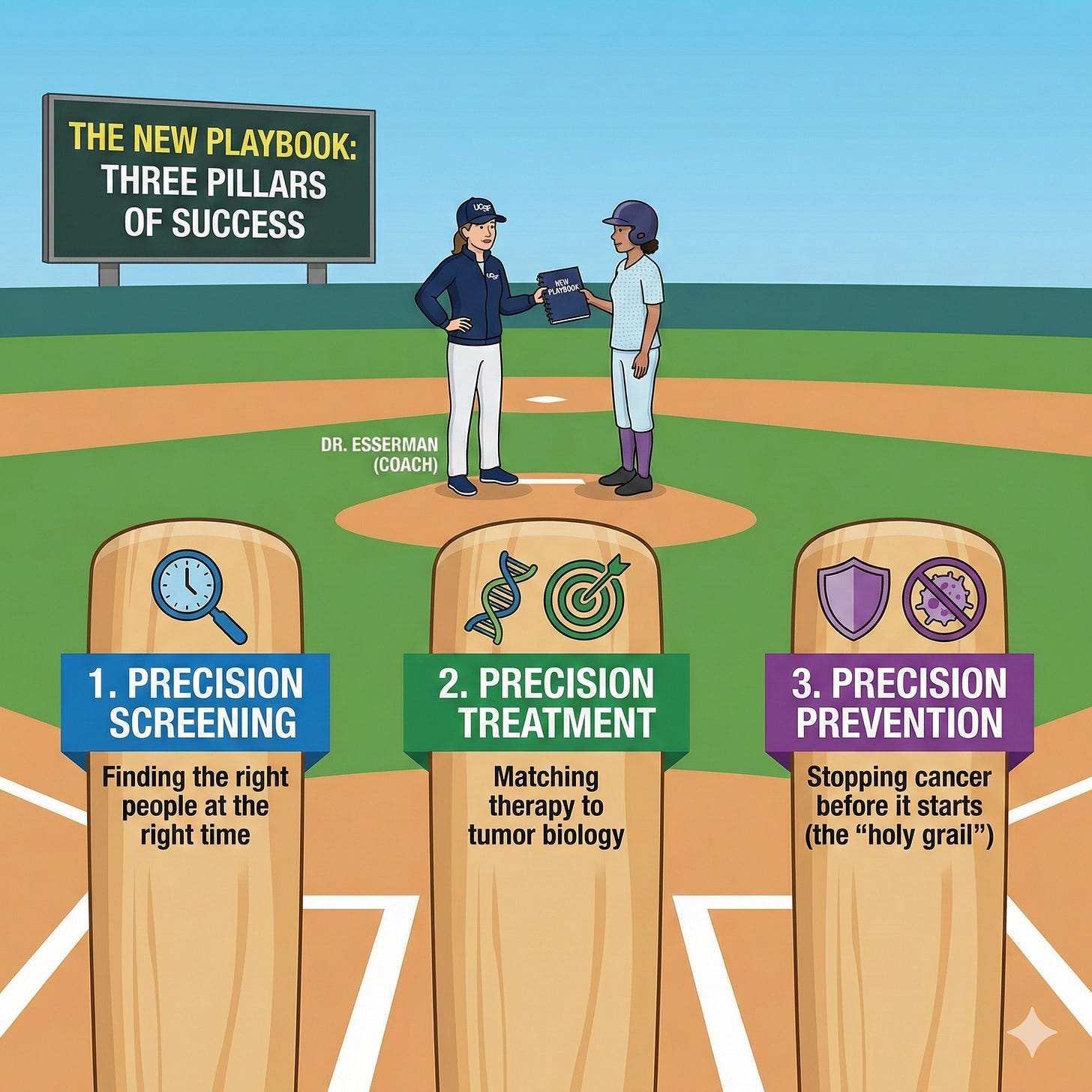
The Prevention Paradigm: Three Precision Tools
The WISDOM study proved risk-based screening works. Zero women in the highest-risk group screened every six months developed stage 2B or higher cancers. That’s precision screening.
But Dr. Esserman isn’t stopping there. She’s pursuing what she calls the three pillars of precision medicine:
Precision screening (finding the right people at the right time)
Precision treatment (matching therapy to tumor biology)
Precision prevention (stopping cancer before it starts)
We already have tools sitting on the shelf that could cut breast cancer risk in half for high-risk women with hormone-positive breast cancers. Tamoxifen. Baby Tamoxifen (a quarter of the dose). These aren't experimental drugs—they're proven interventions most women have never heard of
And they’re just the beginning.
Repurposing What Already Works: The Anti-Progestin Opportunity
Dr. Esserman’s thinking shifted when she realized how often medicine intercedes in women’s health for other reasons: cycle control, birth control, endometriosis, fibroids, IVF, post-menopausal hormone replacement, and osteoporosis.
“Why are we not doing this with an eye towards breast cancer risk reduction?” she asked.
We know progesterone increases breast cancer risk. Anti-progestins should reduce it.
Drugs like Mifepristone and Ulipristal Acetate are already being used to treat fibroids and endometriosis. Early research suggests they could also reduce breast cancer risk. Some researchers are currently testing these agents.
Dr. Esserman’s challenge to the field:
“Why can’t we build a contraceptive that reduces breast cancer risk? Wouldn’t that be amazing? That’s the way to get rid of breast cancer. I don’t want to just keep treating it. I want to prevent it altogether.”
The same logic applies to hormone replacement therapy. We’re redesigning formulations, testing new approaches, and determining what works and what doesn’t. Instead of treating these interventions as separate from cancer prevention, what if we integrated prevention into the design from the start?
The GLP-1 Connection and Other Emerging Links
At last year’s Rise Up conference, one session caught my attention: the connection between GLP-1 drugs (like Ozempic and Wegovy) and breast cancer risk reduction.
This year, there’s a full session on it.
Why? Because the data is starting to show something compelling. Weight loss drugs might do more than help people lose weight—they might also reduce cancer risk.
The same goes for fatty liver disease. Treating it could drop your breast cancer risk. The connections run deeper than we thought.
Dr. Esserman wants to establish an intermediate endpoint framework similar to the one used in cardiology. They conducted nationwide studies to identify risk factors, including blood pressure and cholesterol. Then they proved that lowering those markers reduced heart attacks. Now, if you want to test a better drug, you just measure blood pressure or cholesterol reduction.
“It’s time for us to do that in breast cancer,” she said. “We can develop imaging tests, different ways of doing this. We need to stop saying we can’t do it and say we can do it.”
Heart disease used to be the biggest killer of women. Now it’s cancer.
“I have envy,” Dr. Esserman said. “I want to make that change. I know we can do it.”
The February Moment: Rise Up for Breast Cancer and Women’s Health
On February 19-21, 2026, Dr. Esserman is gathering researchers, OB-GYNs, primary care physicians, and breast cancer specialists at UCSF for the Rise Up for Breast Cancer and Women’s Health Conference.
This isn’t a typical medical conference. The goal is to break down silos—breast cancer researchers don’t always talk to OB-GYNs, OB-GYNs don’t always know enough about risk, primary care doctors aren’t always connected to the latest prevention research.
Rise Up brings them together.
What’s on the agenda:
GLP-1 drugs and breast cancer risk reduction—a full session on what we’re learning about weight loss medications and cancer prevention
Hormone replacement therapy safety—is it safe? Is it not safe? Can you take it after breast cancer? What about the new formulations?
Fatty liver and metabolic connections—how treating one condition might prevent another
Exercise, weight loss, and medication interventions—what actually reduces risk and by how much?
The Spark Awards—funding for researchers with breakthrough ideas for prevention tools and drugs
“All of women’s health is related,” Dr. Esserman explained. “Trying to reduce the risk from fibroids—those medicines will also reduce the risk of breast cancer. There’s so many incredible connections.”
Who should attend? Anyone interested in women’s health innovation. Researchers. Clinicians. Advocates. Patients who want to understand the cutting edge of prevention science.
You can register at riseup.ucsf.edu. There’s also a luncheon to raise money for the Spark Awards—supporting scientists with the boldest prevention ideas.
The Abortion Connection: Reproductive Health and Cancer Prevention
Dr. Esserman wasn’t planning to start a conference focused on reproductive health and breast cancer. But in 2021, when states began criminalizing abortion, she couldn’t ignore the contradiction.
“Here we are trying to save women’s lives from breast cancer when there are so many easy ways to prevent people from dying from completely unnecessary complications because they can’t get access to an abortion when they need it.”
The numbers are stark: One million women experience miscarriage in the U.S. every year. About 20% need a D&C or abortion to prevent complications. If abortion were illegal everywhere, 200,000 lives would be lost annually—five times the number who die from breast cancer.
But it’s not just about access to abortion. It’s about recognizing that reproductive health and cancer prevention are interconnected.
Many of the drugs used for contraception, cycle control, and hormone regulation could be designed with breast cancer prevention in mind. We’re just not thinking about it that way yet.
Dr. Esserman wants to change that.
What’s Blocking Progress: The $4-5 Million Gap
Here’s the frustrating part: Dr. Esserman knows how to do seven years’ worth of work in one year if she has the resources.
The WISDOM study proved risk-based screening works. Now she needs to keep enrolling patients while waiting 1-2 years for insurance guidelines to change.
WISDOM 2.0 is already designed. It includes:
Population-based screening starting at age 30
Updated tools to predict who’s at risk for triple-negative breast cancer based on race and ethnicity
AI algorithms for breast density that identify the actual 10% who need supplemental screening (not the 50-60% currently being over-screened)
New risk reduction interventions being tested in real-time
However, the entire WISDOM study was funded through philanthropy because insurance does not yet cover genetic testing for prevention. They need $4-5 million to bridge the gap until coverage kicks in.
“I don’t want to close the trial to enrollment until I wait for the guidelines to change,” Dr. Esserman said. “I don’t have patience to wait.”
Neither should we.
Your Role in This Future
Dr. Esserman’s vision sounds ambitious. Dropping breast cancer diagnoses from 330,000 to 150,000 per year. Cutting deaths from high-risk cancers by a third. Building prevention tools that make breast cancer rare instead of common.
But here’s what makes it different from typical “moonshot” declarations: She’s not asking for a miracle. She’s asking for resources to scale what already works.
Here’s how you participate:
Join WISDOM if you’re between 30-74 and haven’t had breast cancer. It’s free, mostly online, and your participation helps prove what prevents cancer. (thewisdomstudy.org)
Support the funding gap. WISDOM needs $4-5 million to keep enrolling patients while waiting for insurance guidelines. (giving.ucsf.edu/fund/wisdom)
Demand genetic testing. Genetic testing is cheaper than a mammogram now. You only do it once. And 30% of mutation carriers have no family history—so family history alone isn’t enough.
Talk to your doctor about risk reduction. If you’re high-risk for hormone-positive breast cancer, medications like Tamoxifen could cut your risk in half. These conversations aren’t happening nearly enough.
Attend Rise Up (Feb 19-21, 2026) if you’re a clinician, researcher, or seriously interested in prevention science. This is where the future is being built.
The Key Question
When I asked Dr. Esserman for her advice to anyone who wants to kick cancer’s ass, she didn’t hesitate:
“Get educated, get informed. If you don’t have cancer, join WISDOM. Help me raise money so I can keep this study open.”
Then she said something that’s stayed with me:
“It’s not an emergency, right? But everyone has the time to learn and learn about their own risk and learn about what they can do. Don’t be afraid because you either have the risk or you don’t. Better to be forearmed. Forewarned is forearmed.”
We have the tools. We have the science. We have a surgeon who’s trying to work herself out of a job by preventing the cancers she’s trained to treat.
What we need now is the will—and the resources—to make it happen.
Support the WISDOM Study: giving.ucsf.edu/fund/wisdom
Register for Rise Up Conference (Feb 19-21, 2026): riseup.ucsf.edu
Join WISDOM (ages 30-74, free): thewisdomstudy.org
References & Further Reading
WISDOM Study
Esserman LJ, Fiscalini AS, Tice JA, et al. Risk-Based vs Annual Breast Cancer Screening: The WISDOM Randomized Clinical Trial. JAMA. Published online December 12, 2025. doi:10.1001/jama.2025.24784. Full text
University of California, San Francisco. “UCSF Study Finds a Better Way to Screen for Breast Cancer.” December 12, 2025. Read more
WISDOM Study. “WISDOM 1.0 Study Results: Personalized Breast Cancer Screening is Safe and Smarter.” December 16, 2025. Read more
Park A. “A New Study Challenges the Way We Screen for Breast Cancer.” TIME. December 12, 2025. Read more
Tamoxifen for Breast Cancer Prevention
Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90(18):1371-1388. PubMed
American Cancer Society. “Breast Cancer Prevention: Tamoxifen and Raloxifene.” Read more
Batur P, Blixen CE, Moore HC, Thacker HL, Xu M. Menopausal hormone therapy (HT): an update on alternative and complementary therapies. Cleveland Clinic Journal of Medicine. 2006. Read more
Cuzick J, Powles T, Veronesi U, et al. Overview of the main outcomes in breast-cancer prevention trials. Lancet. 2003;361(9354):296-300. PMC
Rise Up Conference
UCSF. “RISE UP for Breast Cancer and Women’s Health Conference.” February 19-21, 2026. San Francisco, CA. Conference website
UCSF. “Ideas to Implementation (I2I) Competition.” RISE UP for Breast Cancer Conference. Competition details
Additional Resources
Join the WISDOM Study (ages 30-74, free enrollment): thewisdomstudy.org
Support WISDOM Research: giving.ucsf.edu/fund/wisdom
Register for Rise Up Conference (February 19-21, 2026): riseup.ucsf.edu
Listen to the full interview with Dr. Laura Esserman on the Kicking Cancer’s Ass podcast:
This is paid subscriber content. Free subscribers received a teaser with key highlights and the podcast link. Paid subscribers get the complete analysis, conference details, and actionable prevention strategies.