What If the Real Threat Isn’t Cancer Coming Back?
Survivorship is more than cancer monitoring
The system that trains doctors failed women on purpose. Not through malice, but through something worse: indifference compounded by fear.
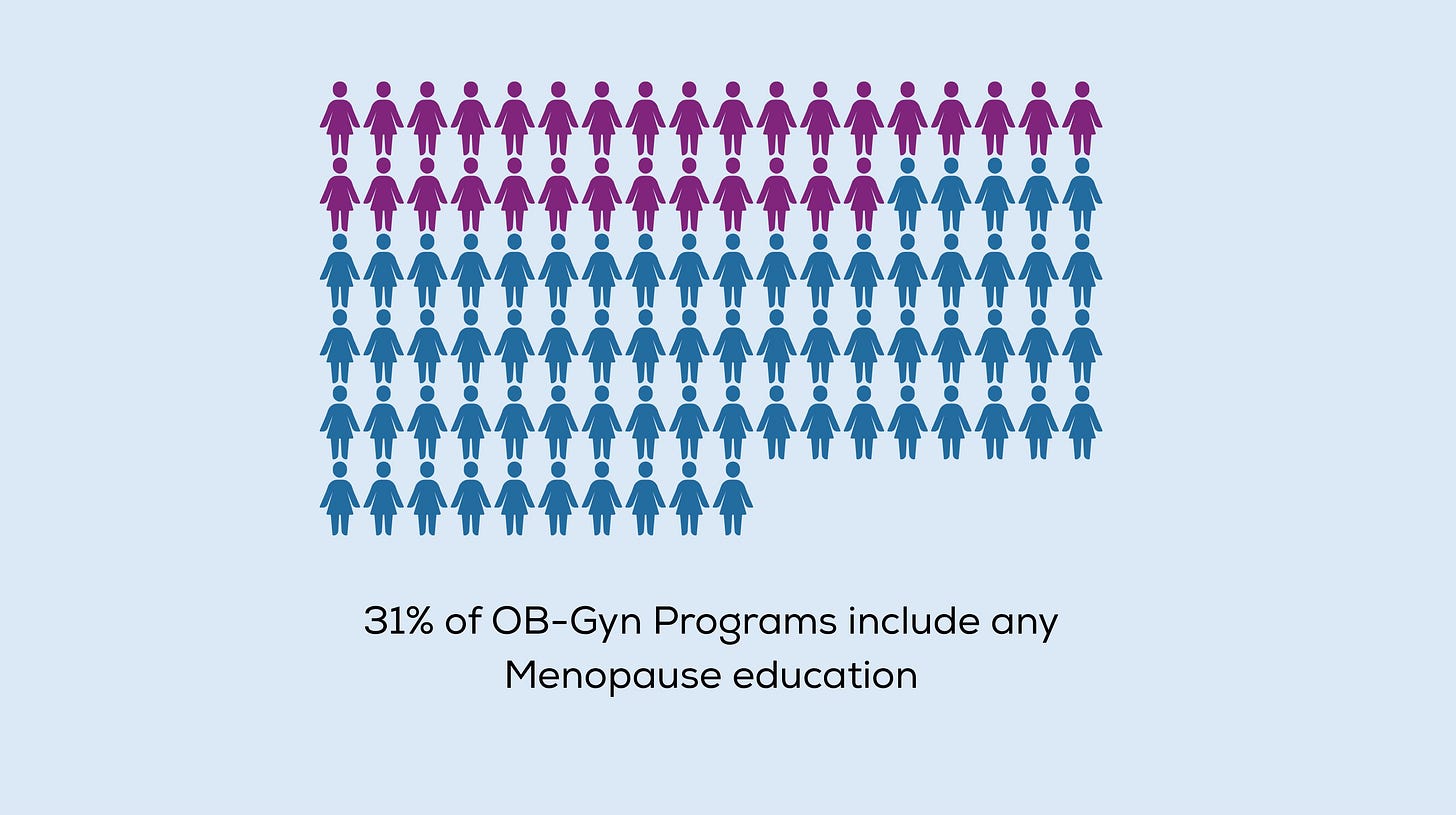
In 2023, only 31.3% of OB-GYN residency program directors reported having any menopause curriculum in their training programs. Think about that. By 2060, approximately 90 million women in the United States will be postmenopausal —spending roughly a third of their lives in this stage. Yet 92.9% of program directors agree residents should have standardized menopause training, while almost none provide it.
Dr. Mindy Goldman chairs the menopause panel for the National Comprehensive Cancer Network. Her career shifted after her best friend died of aggressive breast cancer at a young age—too young for a mammogram, gone within 18 months. When Dr. Goldman returned to work and joined the breast care center, oncologists kept asking her questions: “This patient was thrown into menopause from chemo—what do we do?” She went to find answers in the medical literature. There was almost nothing there.
The gap exists because of what happened 25 years ago. In 2002, the Women’s Health Initiative study was stopped early, and the media exploded with headlines suggesting hormone therapy caused breast cancer. Both doctors and patients panicked. The medical education system responded by essentially erasing menopause from training curricula. If hormones were dangerous and menopause was just “a normal part of aging,” why teach it?
Watch the episode - it can save a life
But here’s what never made headlines: The 20-year follow-up of that same study showed women who took estrogen alone had a 23% lower risk of developing breast cancer and a 44% lower risk of dying from breast cancer compared to women who took a placebo. The harmful component was the synthetic progestin, not the estrogen. Studies since then have shown higher breast cancer risk with synthetic progestins but not with bioidentical formulations, the kind prescribed today.
The correction never reached most doctors. An entire generation of physicians learned to fear hormones. Your oncologist still says no. Your gynecologist says “I don’t feel comfortable, you’re a cancer patient.” Your primary care says “go back to your oncologist.” You’re bouncing between specialists, and none of them can see what Dr. Goldman calls being “lost in the middle.”
Now here’s the cardiovascular reframe that should make you angry:
Heart disease is the leading cause of death for women in the United States. In 2023, it killed 304,970 women—about 1 in every 5 female deaths. Cardiovascular disease kills more women than all forms of cancer combined. Yet only about half (56%) of US women recognize that heart disease is their number one killer.
When you had cancer, everyone focused on preventing recurrence. But what if that’s not actually your biggest risk anymore?
The “timing hypothesis” explains how hormone therapy affects cardiovascular health based on when you start it. Research shows that when hormone therapy is initiated in women younger than 60 or within 10 years of menopause, it significantly reduces both all-cause mortality and cardiovascular disease. The mechanism is straightforward: estrogen keeps coronary vessels healthy and prevents plaque formation. But if you wait until 15 years after menopause, when plaques have already formed, estrogen doesn’t help and might destabilize existing plaques.
Dr. Goldman put it bluntly in our conversation: “It’s not hormone replacement therapy. It’s cardiovascular prevention therapy.”
For cancer survivors, the implications are profound. Many of us were thrown into menopause young through chemotherapy, surgical removal of ovaries, or medications like tamoxifen and aromatase inhibitors. Dr. Goldman explained that when I had my ovaries removed at 38, my body was deprived of estrogen for decades. “That has significant health implications. It can have cardiac and bone density implications. Not to mention the quality-of-life consequences.
The survivorship gap exists because oncologists manage cancer but not menopause. Gynecologists manage menopause but feel uncomfortable treating cancer survivors. The result? You’re told to “be grateful you’re alive” while your cardiovascular risk climbs silently.
So what can you actually do?
First: Understand your specific breast cancer type matters more than you’ve been told.
“Breast cancer is not breast cancer,” Dr. Goldman emphasized. “It is a whole host of different diseases and whether hormones can be used differ depending on the type of breast cancer that someone has.”
If you had hormone-negative breast cancer and remain disease-free for five years, there’s no evidence that hormone therapy increases recurrence risk. For DCIS or non-invasive disease, standard hormone therapy is generally safe. Even for hormone-positive disease—the most common type—the conversation is more nuanced than “absolutely not.”
Second: Ask better questions of your medical team.
Don’t ask “Can I take hormones?” Ask: “Given my specific breast cancer type, treatment history, and cardiovascular risk factors, what does the research show about my options?” Request they consult the NCCN survivorship guidelines Dr. Goldman helped write.
If they dismiss you with “just deal with it,” Dr. Goldman’s advice is clear: “Don’t accept that. Speak to someone who’s an expert and can help you out because there are always, always things that can be done.
Do not accept being told to just deal with the side effects even if you’re in active treatment.”
Third: Know the non-hormonal options that actually work.
Low-dose antidepressants. Gabapentin for nighttime hot flashes. Fezolinetant (Veoza), approved by the FDA in 2023, targets the specific brain neurons where hot flashes occur. Vaginal estrogen, which recent studies show doesn’t impact survival even in breast cancer survivors.
Fourth: Recognize that cardiovascular risk assessment IS survivorship care.
Ask your doctor: “What’s my 10-year cardiovascular disease risk?” If you’re younger than 60 or within 10 years of menopause, and your cardiovascular risk is low to moderate, the timing hypothesis suggests you’re in the window where hormone therapy might reduce your biggest health threat.
The medical system failed to train doctors properly. That’s the system failure. But you don’t have to accept its consequences. That’s the self-advocacy part.
The biggest myth about post-cancer life, according to Dr. Goldman? “That you just have to deal with any of the side effects related to treatment.” You don’t. Exercise regularly—it reduces recurrence risk and improves survival. Push harder when you’re not getting answers. Find specialists who treat the whole person, not just the cancer history.
What if the real power move isn’t fighting cancer harder—it’s reframing what survival actually means? You didn’t come this far to spend the next 30 years suffering through preventable cardiovascular disease while everyone congratulates you for being cancer-free.
Reflection questions:
When was the last time a doctor assessed your cardiovascular risk as thoroughly as they assess your cancer recurrence risk?
If hormone therapy might reduce your leading cause of death, what questions do you need answered to make an informed decision?
What would survivorship care look like if it treated your whole body’s needs instead of just monitoring for cancer?
RESEARCH CITATIONS & LINKS
Medical Education Gap Statistics
31.3% of OB-GYN programs have menopause curriculum:
Source: Allen JT, et al. “Needs assessment of menopause education in United States obstetrics and gynecology residency training programs”
92.9% of program directors agree residents need standardized menopause training:
Same source as above
90 million US women will be postmenopausal by 2060:
Source: Contemporary OB/GYN survey report
Women’s Health Initiative Study - Corrected Findings
Estrogen alone: 23% lower breast cancer incidence, 44% lower breast cancer mortality (20-year follow-up):
Source: Chlebowski RT, et al. “Twenty-Year Follow-Up of Women’s Health Initiative Trials”
Links:
Bioidentical progesterone vs synthetic progestins:
Source: “Estrogen-alone Therapy and Invasive Breast Cancer Incidence” (WHI Observational Study)
Cardiovascular Disease Statistics
Heart disease killed 304,970 women in 2023 (1 in 5 female deaths):
Source: CDC - About Women and Heart Disease
Link: https://www.cdc.gov/heart-disease/about/women-and-heart-disease.html
CVD kills more women than all forms of cancer combined:
Source: Go Red for Women / American Heart Association
Link: https://www.goredforwomen.org/en/about-heart-disease-in-women/facts
Only 56% of US women recognize heart disease as their #1 killer:
Source: CDC - About Women and Heart Disease
Link: https://www.cdc.gov/heart-disease/about/women-and-heart-disease.html
Timing Hypothesis Research
Hormone therapy initiated in women <60 years or within 10 years of menopause reduces all-cause mortality and cardiovascular disease:
Source: Hodis HN, Mack WJ. “Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease”
Links:
Timing hypothesis overview (window of opportunity):
Source: Clarkson TB, et al. “Timing hypothesis for postmenopausal hormone therapy”
After 15 years postmenopause, hormone therapy may destabilize existing plaques:
Source: Multiple studies on timing hypothesis
New Treatment Options
Fezolinetant (Veoza) - FDA approved, targets specific neurons:
Source: Multiple news sources reporting on FDA approval
Note: FDA approval was May 2023, confirmed in Dr. Goldman interview transcript
Additional Background Research
WHI Study full details:
JAMA publication: https://jamanetwork.com/journals/jama/fullarticle/2768806
NCI analysis: https://www.cancer.gov/types/breast/research/ert-benefits-risks-age
Cleveland Clinic review on timing hypothesis and cardiovascular risk:
Susan G. Komen overview on menopausal hormone therapy and breast cancer:
Note: All statistics and research findings cited in the article come from peer-reviewed publications in journals like Menopause, JAMA, and government sources like the CDC. These are the same sources Dr. Goldman references in her clinical guidelines work with the National Comprehensive Cancer Network.