Waiting (on deck)
Patience is not my virtue
Waiting is constant in the batter's box. The pitcher controls the tempo. I waited for doctors' recommendations - not very long because I was fortunate. Everyone waits to see their doctors. Most of us wait to get an appointment. Leaving a message requesting an appointment requires waiting for a callback. I'm very persistent, but you have to balance persistence with irritation. Most offices will call you back within the day - so you wait with your phone and jump off whatever Zoom call or meeting you might have if the number shows the doctor's office.
You wait for pathology. For the majority of patients, even the most aggressive breast cancers aren't so fast-growing that you must start treatment tomorrow. The exception is inflammatory breast cancer (1-5% of breast cancer diagnoses). I have no experience with that type of breast cancer, and if that's your curveball, suggest Laura Holmes's book, This is Cancer, as she is a practical, articulate, young Stage 4 invasive breast cancer survivor. We can afford to wait until the full pathology is confirmed for the rest of us.
The wait for the pathology is difficult but valuable. There are multiple types of breast cancer - ductal carcinoma in situ (DCIS - non-invasive), invasive carcinomas - both ductal (most common) and lobular, inflammatory, and a few rarer ones. Within invasive ductal breast cancer, there are multiple types depending on what hormones the tumor reacts to. The types are HER+/HR+, HER-/HR+, HER+/HR-, Triple Negative. These hormone receptors determine the treatment plan and the potential pitches you will see and hit. DCIS may require active surveillance, which means doing nothing except twice annual scans to see if it's grown. Invasive HER+ tumors are candidates for Herceptin from Genentec - a low side effect, highly effective treatment. Each combination of pathology and stage has different treatment protocols. One of the hardest things about talking with other breast cancer patients is that the treatment loops, with their side effects and challenges, are very distinct for each cancer.
I wanted to know what my treatment loop was going to look like as my strongest impulse under stress is to take control. I knew I was not in control. And for a few days, I didn’t’t know who was in control, which was very unsettling.
At my first meeting with my UCSF team, they had the pathology from the other hospital (Sutter) and the scans (MRIs) from January and June. They didn't have the PET scan results because I abandoned the wet read. My first meeting with my extraordinary team was filled with caveats. As long as the PET scan is clear…. As long as the UCSF lab confirms the pathology…. There's less than a 5% chance something will be on the PET scan. The UCSF team did know that the tumor was aggressive and that there was no sign of it in June. Since June, it had developed and invaded a lymph node. Spry fucker.
I remember hearing 5% probability and experiencing my rational mind arguing with my emotional mind in cycles until I was called about the PET scan results. Rationally - 5% is a very low probability. Rationally - there was no cancer in the biopsies done on the tissue removed in October during my breast reduction. Rationally - there's nothing there. Emotionally - what if? This tumor is very aggressive and grew so fast that the doctors thought it was cool. What if it took off through my body, and the PET scan reveals we have a bigger problem? What if my metabolically active tumor doesn't have an appetite for chemo, and it doesn't work? What if my body cannot withstand the onslaught, and we have to stop or pause cycles, and that lets this very aggressive tumor gain a permanent foothold. Rational brain - seriously, Joelle, 5%. Keep perspective. It's hard to do when you are in the box waiting for the pitch.
The PET Scan Results were in that evening, and Dr. Esserman's office called to let me know I was all clear. One tumor…with a lymph node but no sign of cancer outside of that spot. The best possible answer. And the rhythm of the treatment loop became clear because she prescribed low-dose, weekly Carbo-Taxol for 12 cycles. If my tumor didn't fully respond with a Clinical Complete Response (CCR), I would then receive Adriamycin Cytoxan (AC) every two weeks for 4 cycles. At that point, irrespective of Complete Clinical Response, surgery would follow.
Because I was BRCA 1, the only recommended surgical option was a bilateral mastectomy. For people with my pathology who do not have a genetic marker, there can be an option of a lumpectomy. Having already decided to have a bilateral mastectomy before I had cancer, I was not saddened by the surgical direction. But that's because I already had grieved losing my breasts as I decided and prepared for the prophylactic procedure. Cancer gave me four more months with them than I expected.
More waiting. And during the waiting, it is very, very hard to focus on anything other than "I have cancer, and it's still growing inside me." From Dr. Chien to the first treatment, I waited two weeks. The wait was a combination of a second pathology review, port placement (which can be done concurrent with the first chemo, but I had two weeks, so no need), and securing a seat with Dignicap machine in a UCSF infusion center - weekly on Tuesdays or Wednesdays so that my infusions were the same days as Dr. Chien's clinic - preventing additional trips to the hospital. By the way, that was Dr. Chien's idea, and it was excellent. Combined with my minimal side effects, I was able to box cancer into one day a week most weeks.
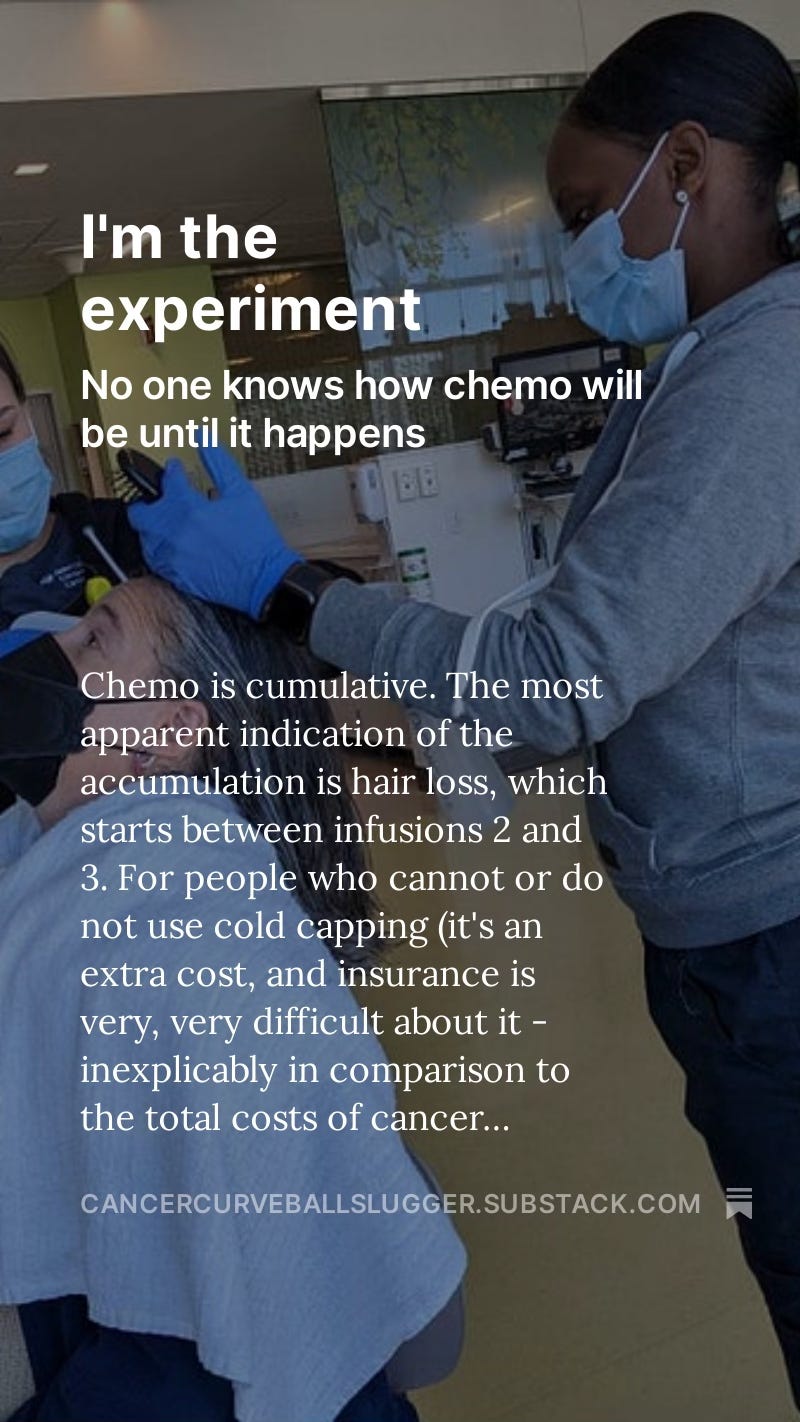
Next is waiting for the first infusion. No one knows how their body will respond to the poison of chemo until the first cycle of receiving the stuff. Tremendous strides have been made to reduce side effects with pre-treatments.
I knew that the side effects from chemo can be disabling because I lived through that with my sister's experience of AC. And I knew there was a class of drugs that dramatically reduced the nausea and vomiting. I asked Dr. Chien if Emend (Aprepitant) could be part of my pre-treatment. She asked how I knew about that, mentioned it wasn't usually needed for Carbo-Taxol, and agreed to prescribe it. She recommended a cousin of Emend - Cinvanti - as she finds it more effective. My insurance decided to cover it, which was part of every infusion. Knowing I had Cinvanti on board made me much less anxious about the first infusion, but the waiting was hard.
During the waiting, I used the time to prepare. Again - my stress response is to take control. My self-soothing is through action. Action gives me both pride of accomplishment AND a feeling of control. That's only right for some, but it helped me. Here are ten things I did during the waiting for the first infusion.
Found Sadie, my psycho-oncologist, and began working with her. I interviewed three possible therapists for this role.
Received and tried on my sister-in-law's chemo tops with zippers to access the port. She also sent her wigs. I still haven't taken the wigs out of the box.
Ordered the Dignicap kit with enough time for it to be delivered.
Ordered new slippers just for the infusion center.
I wanted an aromatherapy option that would be relaxing for me but wouldn't bother my fellow chemo patients. A shop that sells essential oils recommended a personal aromatherapy locket. I found it on Amazon, and it worked perfectly.
I ordered ice socks and mittens and froze the ice packs and the additional ones gifted to me.
Asked my sister to borrow her Yeti cooler for the ice packs.
Put together my Cancer Obliteration Project binder (I'll share the structure in an appendix to the book) that would come to every infusion and doctor's appointment.
Picked up all prescriptions and tried to organize them for when I needed them.
Found and set up an app (Max) that would alert me when it was time to take an anti-emetic so that I would stay ahead of the nausea and pain.
I was as organized as possible for my first infusion.
Finally, the first infusion day arrives. More waiting.
Check in for the lab draw - and wait.
Check vitals. Blood pressure elevated because I’m anxious. Breathe. Mindfulness. Blood pressure lowers. Get the lab draw.
Check in for my oncology appointment. Wait.
Get the results on your MyChart and have yet to learn what they mean. Looks like green means good.
The medical assistant brought me back to the doctor's clinic. Recheck vitals. Ask about any new allergies or other new developments. Very pleasant. Please change into a gown. Wait.
The nurse practitioner reviewed the chart, checked everything, and examined me. Wait.
Then, the doctor checks the chart, describes what happens next, and examines me. I feel better because the labs are good, and she is encouraging.
Get dressed. Check-in for the infusion. Wait.
Called back into the infusion center.

Quick tour - here's the bathroom. Here's your seat and the Dignicap machine. Can I get you a warm blanket and anything to eat or drink? Warm blankets are very nice. The chairs are comfortable recliners. Mom sits across from me with the Yeti cooler as her footrest. We wait.
We read while we waited.
Eventually, when the infusion center knows the chemo medicines are being mixed by the pharmacy, the pre-treatment begins. The pre-treatment is timed to help with reactions to the chemo as it's infused, and for 48-72 hours, it's in your body. So you wait until the time is right. Then it begins.
I hate the wait. I don't idle well. I have to work very hard to still my mind during the wait and divert my focus from the what might happen disaster prophesying. This wasn't new information, but I only realized so much of treatment is waiting. The job I had given Taylor to write me weekly gave me one thing to do during the wait - I'd read his letter. My friend Julian inevitably and intentionally texted me every chemo day - so our playful banter distracted me during the wait. My Rabbi Rebecca Schatz pulled together prayers and songs I could say and play (all on YouTube, and I conveniently made a playlist), which helped a lot during the wait. Heather recommended downloading TV shows - which I tried, but I found that I preferred the banter, music, and letters. I had someone with me for every chemo, which created opportunities to get to know a few people better (Julie and Molly) and to share time with people I already knew and loved. They were all part of distracting me during the wait. All the distractions made me happy, and I decided it was good to let myself feel satisfied as I faced my chemo days and even to think of my chemo days, the treatment loop, as a countdown. 1 down, 11 to go. That slight shift was my initial defense against my internal, but what about dialogue.
Continue the story…


I'm really engaged in your story, Joelle. You've written every detail and I'm sure it will help others as they read your book for inspiration and practicality.