Three Lies About Sex and Cancer Your Medical Team Won’t Correct
Cancer And Your Sex Drive
My nurse practitioners told me I’d need condoms with my husband after my cancer diagnosis.
We’ve been married since 1998. Monogamous. The whole nine yards. But there I was, six weeks into treatment, dutifully using condoms because that’s what my medical team told me to do.
My sister finally asked: “Did you ask if it’s about pregnancy prevention or chemo risk?”
I hadn’t asked. Turns out, it was just pregnancy prevention. I have no ovaries. If I get pregnant, it’s the Messiah.
That was the extent of my “sex after cancer” conversation with my medical team. Unnecessary condoms and nothing about desire, pain, atrophy, or what happens when hormone blockers steal what clinical sexologist Richelle Menzies calls your “sparkle.”
87% of cancer patients report sexual dysfunction during treatment. Only 27% are ever asked about it.
This week on Kicking Cancer’s Ass, I sat down with Richelle Menzies, USA Today bestselling romance author Cara Lockwood, and pharmacologist Dr. Erika Reith—all breast cancer survivors—to break the silence. What emerged wasn’t just a conversation about sex. It was a dismantling of three core lies that keep women suffering in isolation.
Get the full episode: Apple | Spotify | YouTube
Lie #1: You Won’t Want Sex During Treatment
The night before my breast reduction surgery—years before my cancer diagnosis—I lay in bed grieving. I knew the surgery meant losing sensation in the lower part of my breasts. That area had been a significant part of my sexual pleasure, and I had no idea what intimacy would look like after.
When cancer hit, I lost even more. But here’s what nobody told me: some days, you’ll actually feel frisky.
“I talk about my sparkle and I just felt like hormone blockers took my sparkle,” Richelle told me. “That cognitive side of it, the lack of desire, feeling just fatigued—during cancer treatment, it was like the last thing that I wanted to do.”
She’s right about the fatigue, the hot flashes, the hormone crash. But she’s also right about something else: it’s not constant.
Every day is different. Some days you won’t want to be touched. Some days you’ll want to be held. And some days? You might actually want sex.
When I asked what she wished someone had told her, Dr. Erika Reith said: “Nobody talks to you about what it’s going to feel like.”
The medical system treats your sexuality like an optional feature that can be turned off for the duration of treatment. But your body doesn’t work that way. You’re not a machine entering maintenance mode.
Cara Lockwood put it best: “Cancer doesn’t get to decide that you don’t like sex anymore. That is not cancer’s job. It doesn’t get to take that from you. It’s still in your control, in your power.”
If you feel good enough to want intimacy, indulge it. Those moments release oxytocin, serotonin, all the happiness hormones your body desperately needs. Sex isn’t frivolous during cancer treatment—it’s medicine.
Lie #2: Your Body Is Broken and Won’t Work the Same
When Cara got her reconstruction, everyone told her how lucky she was. “Now they’re bigger. Now they’re perkier.”
She wasn’t excited.
“They weren’t mine,” she said. “They felt alien. I still had a lot of memories of pain. The loss of sensation hit harder than I expected. Nobody in the medical system thought to warn me.”
This is where the medical establishment fails spectacularly. They focus on the mechanics—surgery recovery timelines, wound care, radiation schedules—but not on how you’ll feel about your body afterward.
Richelle’s experience was even more extreme. “I had got to the point where even washing myself was painful. Externally, my clitoris had shrunk. I couldn’t orgasm. Any touch was hell. It had progressed to that point where touching, washing myself, just my clothes touching my vulva was awful.”
Your body isn’t broken. It’s responding to a cascade of hormonal changes that crash your estrogen, tank your testosterone, and create vaginal atrophy so severe that intimacy becomes genuinely painful.
But here’s what nobody tells you in the oncology office: there are remedies.
Dr. Erika Reith walked through the complete intervention hierarchy:
Start with use: “The more you use your equipment, the better lubricated your equipment can be, the better the blood flow.” But she added a critical caveat—if there’s pain, deal with the pain first. Don’t condition your body to associate touch with suffering.
Vaginal moisturizers: Hyaluronic acid suppositories, Replens, Revaree. Non-hormonal options that replenish moisture.
Vaginal estrogen: This is the game-changer. Richelle was so desperate she didn’t even ask her oncologist—she just started using it and brought the research to her next appointment. “I was straight back using it. When I went in, I went, ‘Right, I’ve started using this and here’s the research.” The research now shows vaginal estrogen is safe even for hormone-positive cancers. It’s localized, it works, and it can reverse severe atrophy.
Testosterone: For women in their 30s and 40s who had good libido before treatment, testosterone can restore energy within one week and libido within three months. “As a woman in my 30s who had a good libido prior to cancer, quality of life is very important,” Dr. Reith said. “You have to make those individual decisions for yourself with your care team.”
Richelle’s colleague from her first menopause put her on testosterone cream after blood work showed her levels were at zero. “Within like a week, my energy levels had improved. It took about three months for the libido to kind of kick back in.”
Your body can work. It just might work differently. And there are medical interventions that can help you reclaim what cancer tried to take.
Lie #3: You Shouldn’t Prioritize Sex and Intimacy During Treatment
My husband, Neal, assured me he found all of me sexy. He was so relieved my cancer was caught early that nothing else mattered. But he also started treating me like I was fragile. He became tentative—what did I feel like? Could he touch me?
I wanted to be seen as a sexually desirable creature, not just a cancer patient.
We had to talk about exploring other ways to excite each other because we’d lost one that had been significant. And we had to keep talking—every day brought something different.
“The key to everything is good communication,” Cara said. “Part of that is being honest with yourself about what it is you like and what it is you don’t like.”
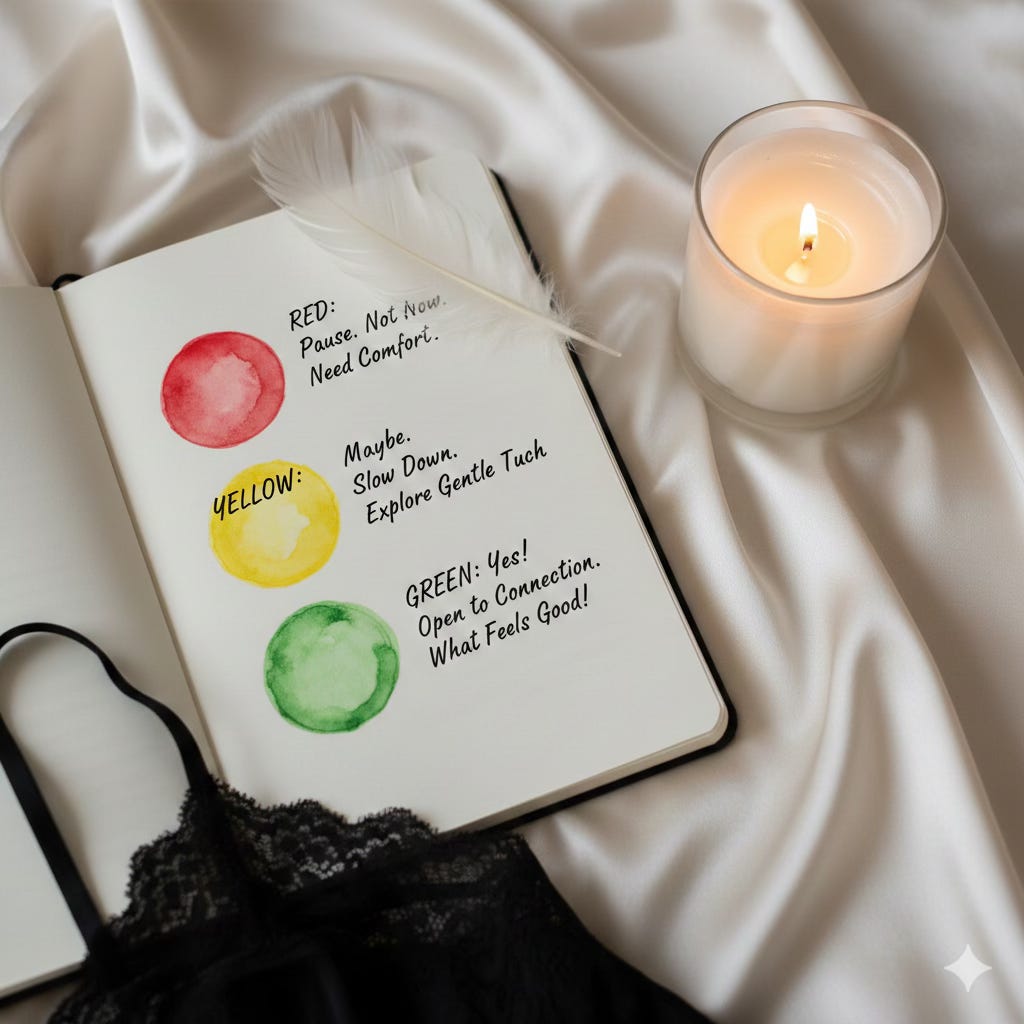
Richelle uses a traffic light framework with her clients:
Red: Things you definitely don’t want
Yellow: Nice to have but not essential
Green: Your needs, your must-haves
Do this for yourself first. Sit down with a piece of paper and actually write it out. Then have the conversation with your partner.
“Once you’ve done that for yourself, then you can talk about it,” Richelle explained. “It’s a great negotiation tool. Otherwise, there’ll be lots of ‘what do you think about this? I don’t know’ because you haven’t had that time to sit and reflect.”
But communication isn’t just about negotiating what you can’t do. It’s about permission to explore.
Richelle told the story of Christopher Reeve, paralyzed from the neck down, whose wife discovered one spot on his shoulder that gave him intense pleasure. That became his erogenous zone. “You will often see me standing next to him with my hand on his shoulder,” his wife said in an interview.
“The brain and the body can do such amazing things,” Richelle said.
Dr. Reith dated after treatment and had to navigate intimacy with someone new while still figuring out her post-cancer body. “It’s like discovering your sexuality for the first time,” she said. “Whoever you were sexually before, you cannot expect to return to exactly that person. But it just might look and feel different than before.”
This is where Cara’s advice becomes essential: “It’s an opportunity to re-explore that person, to talk about things that you haven’t talked about. Maybe there’s that thing you actually never liked. You can finally say, ‘And especially now, I don’t like that. But I really do like this other thing.’”
What Your Oncologist Should Tell You (But Probably Won’t)
At the end of our conversation, I asked each of them what advice they’d give to someone looking to reclaim their intimate life after cancer.
Cara: “Cancer doesn’t get to decide that you don’t like sex anymore.”
Richelle: “Your body, your choice. Medical professionals don’t get to decide either.”
Dr. Reith: “Commune with the part of yourself that still knows how to be well. Imagine yourself in the state of wellness that you want, in the sex life that you want.”
Here’s mine: If you feel good enough to want intimacy, indulge it. It’s more than okay. It’s good for you.
There’s a continuum. If your sparkle’s out, that’s okay. If you feel frisky, that’s okay too. But most importantly, whatever side effects you’re having—and there may be many—there are likely remedies to mitigate them.
You just have to ask for them. Demand them.
The Questions to Ask Tomorrow
Don’t wait for your oncologist to bring this up. They won’t.
Ask your oncologist:
“How might this treatment affect my sexual function, and what interventions are available?”
“Is vaginal estrogen safe for my specific diagnosis?”
“Can you refer me to a sexual health specialist or survivorship program?”
Ask your OB-GYN:
“What can you prescribe for vaginal atrophy and pain during intercourse?”
“Should we consider testosterone therapy given my hormone levels?”
Ask your nurse navigator or social worker:
“Who can I talk to about sexual health during treatment?”
“Are there specialists who work specifically with cancer patients on intimacy issues?”
If one provider doesn’t have answers, keep asking. Nurses often have more practical knowledge than doctors. OB-GYNs who specialize in survivorship care know more than general practitioners. Sexologists who’ve been through cancer themselves understand both the medical and emotional landscape.
Don’t accept silence as an answer.
You Are Not Your Cancer
Sex during cancer treatment isn’t about performance or maintaining some pre-diagnosis standard. It’s about connection, pleasure, and remembering that you’re still you.
Some days you’ll want to be held. Some days you won’t want to be touched at all. And some days, you’ll want the reminder that your body can still feel good, that intimacy is still possible, that cancer hasn’t stolen everything.
Those days matter. Your pleasure matters. Your intimacy matters.
Don’t let anyone—not your medical team, not well-meaning friends, not even your own fear—convince you otherwise.
Get the full episode: Apple | Spotify | YouTube
Resources mentioned in this episode:
Come As You Are by Emily Nagoski (understanding responsive vs. spontaneous desire)
A Better Normal (redefining sexuality after cancer)
Get the full episode: Apple | Spotify | YouTube
Richelle’s Libido Recovery Masterclass with a discount
Libido Recovery Masterclass (for couples)
Course
61 Lessons
CURRENTLY 75% off! (Full price, $997USD). An online program for couples to recover affection and desire after treatments. Through education, practical and fun activities (and a bit of neuroscience), libido and intimacy can be recovered. For all partnerships impacted by cancer, wanting things to get back to the way they used to be.
https://atouchysubject.podia.com/libido-recovery-for-couples-6-weeks/3x102
RESEARCH LINKS
VAGINAL ESTROGEN SAFETY & EFFICACY:
JAMA Oncology 2023 Study - No increased breast cancer mortality with vaginal estrogen:https://jamanetwork.com/journals/jamaoncology/fullarticle/2811413
Breastcancer.org Summary - Vaginal estrogen safe for women with breast cancer:https://www.breastcancer.org/research-news/vaginal-estrogen-safe-for-women-with-breast-cancer
PubMed - Systematic Review - Safety of vaginal hormones in breast cancer survivors:https://pmc.ncbi.nlm.nih.gov/articles/PMC10704880/
ACOG Clinical Guidance - Treatment of urogenital symptoms in breast cancer survivors:https://www.acog.org/clinical/clinical-guidance/clinical-consensus/articles/2021/12/treatment-of-urogenital-symptoms-in-individuals-with-a-history-of-estrogen-dependent-breast-cancer
2025 Meta-Analysis - Vaginal estrogen use and recurrence/mortality risks: https://www.ajog.org/article/S0002-9378(24)01126-8/fulltext
TESTOSTERONE THERAPY FOR WOMEN:
Testosterone Implant Research - Benefits in breast cancer survivors:https://www.liebertpub.com/doi/10.1089/andro.2021.0003
Testosterone & Quality of Life - Improvement in all domains (depression, fatigue, joint pain, libido):https://valleyhealthspan.com/testosterone-therapy-for-breast-cancer-survivors/
Topical Testosterone Safety Study - No estradiol elevation with testosterone gel: https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-024-01886-7
ASCO Educational Book - Enhancing sexual health for cancer survivors:https://ascopubs.org/doi/10.1200/EDBK-25-472856
HEALTH BENEFITS OF SEX & INTIMACY:
Cleveland Clinic - 5 benefits of a healthy sex life (oxytocin, endorphins, immune function):https://health.clevelandclinic.org/benefits-of-sex
WebMD - 10 surprising health benefits of sex (stress reduction, pain relief, immune boost):https://www.webmd.com/sex-relationships/sex-and-health
Healthline - The health benefits of sex (IgA antibodies, oxytocin bonding):https://www.healthline.com/health/healthy-sex-health-benefits
Harvard Health - Oxytocin: The love hormone (stress/anxiety reduction): https://www.health.harvard.edu/mind-and-mood/oxytocin-the-love-hormone